



However, veno-venous (VV) ECMO was first instituted for patients with septic shock associated with acute respiratory failure, with a ratio of arterial oxygen tension to inspired oxygen fraction (PaO 2/FiO 2) 0.5 µg/kg/min).
Veno-arterial (VA) ECMO was indicated for patients with acute circulatory failure and a systolic blood pressure 0.5 µg/kg/min), and in those with in-hospital cardiac arrest >10 min in duration despite cardiopulmonary resuscitation (CPR). ECMO was implemented for patients in whom the aetiology of septic shock was considered potentially reversible by physicians. We followed the recommendations of the Surviving Sepsis Campaign guidelines when diagnosing and treating septic shock ( 13, 14). We retrospectively reviewed data from 37 patients (aged ≥18 years) with septic shock who underwent ECMO at Hallym University Sacred Heart Hospital between January 2007 and September 2015. In the present study, we hypothesised that the early changes in coagulation profiles and lactate levels would be significantly associated with hospital outcomes in patients with septic shock undergoing ECMO and, therefore, that the evaluation of these parameters might be useful to guide physician decision-making in terms of ECMO treatment. Hence, we suggest that ECMO accelerates pre-existing coagulopathy in septic shock patients the extent of coagulopathy would thus differ between survivors and non-survivors from the time at which ECMO support is commenced. However, coagulopathy can also progress in patients undergoing ECMO, which is associated with blood-surface interactions and/or clotting within the ECMO device ( 12). Specifically, several authors have highlighted the importance of the dynamic evolution of coagulation marker levels ( 10, 11).
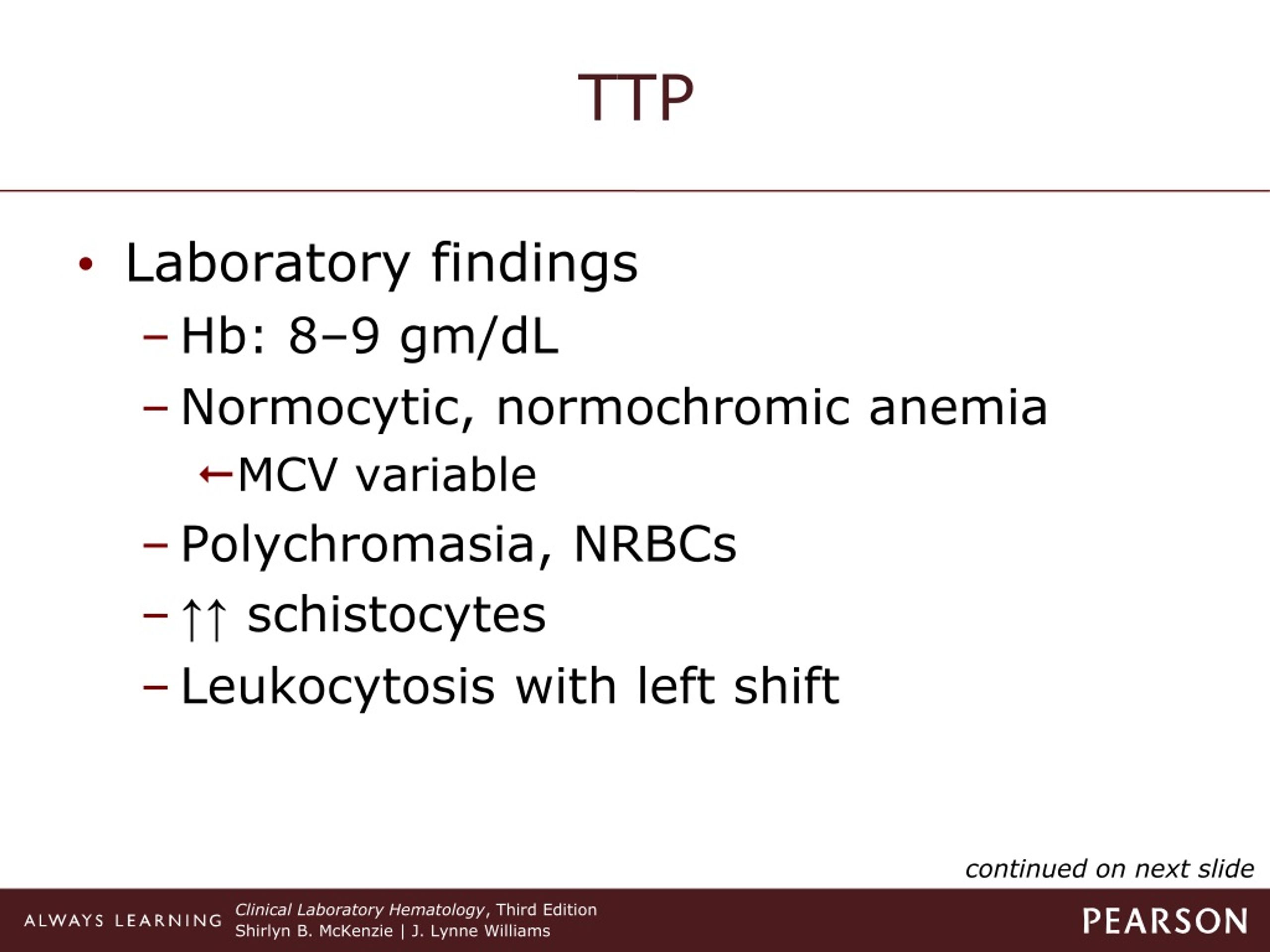
#DIC LAB FINDINGS TRIAL#
Data from a well-controlled clinical trial revealed abnormalities in coagulopathy, inflammation, and the levels of biomarkers of endothelial injury in patients with severe sepsis ( 9). In addition, ECMO is costly ( 6).ĭisseminated intravascular coagulation (DIC) develops in 35% of patients with severe sepsis and is associated with accelerated organ failure ( 7, 8). However, its utility remains controversial in adult patients ( 4, 5). Extracorporeal membrane oxygenation (ECMO) has become a life-saving treatment for neonates and children with septic shock refractory to conventional treatment ( 2, 3). The annual incidence of sepsis, a leading cause of death worldwide, is increasing, and the mortality rate from septic shock is 25–50% ( 1). Keywords: Disseminated intravascular coagulation (DIC) extracorporeal membrane oxygenation (ECMO) lactate septic shock
#DIC LAB FINDINGS PLUS#
Furthermore, the pre-ECMO DIC score plus lactate level was the best predictor of hospital death. 26.7%, P=0.001).Ĭonclusions: During the early period of ECMO support, the coagulation profiles and lactate levels exhibited different trajectories in survivors and non-survivors. Receiver operating characteristic (ROC) curves revealed that the combination of pre-ECMO DIC score plus lactate level was the best predictor of hospital death (area under the curve, 0.879 0.771–0.987) patients with combined scores >9.35 (the optimal cut-off) exhibited a three-fold higher mortality rate than did those with lower scores (81.8% vs. On a multivariate analysis, the pre-ECMO DIC score was significantly associated with hospital death. Additionally, the lactate levels improved considerably in the pre-ECMO non-overt-DIC group and in survivors during ECMO support, but not in the pre-ECMO overt DIC group or non-survivors. However, the DIC scores were significantly higher, at all three time-points, in non-survivors than in survivors. The initial DIC scores did not change in either the pre-ECMO overt-DIC (n=15) or non-overt-DIC (n=22) group after ECMO commencement. Results: A total of 37 patients were included, and 15 (40.5%) patients survived. Methods: A retrospective analysis of coagulation profiles, including disseminated intravascular coagulation (DIC) score, before and during 48 h of ECMO support, was conducted in patients with septic shock undergoing ECMO. Background: To investigate the impact of coagulation profiles and lactate levels in patients with septic shock undergoing extracorporeal membrane oxygenation (ECMO).


 0 kommentar(er)
0 kommentar(er)
